Contraception is concerned with methods or devices that prevent pregnancy, by blocking either the ovum’s fertilisation or its implantation in the uterus in case it has been fertilised.
Choosing the method of contraception depends on several factors, such as:
- the person’s health condition.
- the cycle’s regularity.
- how easy it is to use.
- the side-effects.
The doctor must detail all the available solutions, after he/she judges what may harm a person’s health, based on their previous personal and family history. We must consider that a contraceptive method that is now suitable, may not be so after a certain period of time. What is more, we need to understand that in order for a contraceptive method to be effective, we need to comply with its proper use.
Natural contraceptive methods
Interrupted intercourse
This is one of the most traditional, and common, methods of contraception. There is a high failure rate due to the need for extreme control on the man’s part, but also due to the small amount of pre-ejaculatory fluids that are placed in the vagina during intercourse, before ejaculation takes place.
Irrigation (washing out) after intercourse
There are several liquid preparations for vaginal irrigation right after intercourse. However, 90 seconds after ejaculation has taken place, the cervical mucosa contains sperm which moves on to the uterus. Therefore, this method is unreliable and non-effective.
Natural family planning
1. The calendar method
This method predicts the day of ovulation using the documentation of the cycle’s duration for several months (6–12).
The onset of the fertile period is calculated by removing 18 days from the smallest cycle, while the last fertile day is calculated by removing 11 days from the duration of the largest cycle. If, for example, a woman’s cycles fluctuate from 27 to 32 days, abstinence starts from day 9 (27-18=9) and ends on the 21st day (32-11=21).
2. The cervical mucus method
This is based on observing cervical secretion which is increased during the fertile period. This method requires an extensive observational period before the woman is capable to distinguish between vaginal secretions and cervical mucus.
Abstinence begins on the day of the first indications of cervical mucus and lasts up to 4 days following the largest amount of cervical mucus secretion.
3. The method of temperature measurement
The relationship between ovulation and body temperature is known since 1920. Measurement and recording of temperature is performed daily, via the vagina or the rectum, as soon as the woman wakes up. During ovulation, temperature may rise between 0.3 to 0.4 degrees Celsius and remains high until menstruation begins.
4. Combination of methods
For example, this can be done by combining the calendar method with the temperature method for a more secure result.
5. Lactational amenorrhea (absence of menstrual period)
During exclusive breastfeeding, it is very rare that pregnancy may occur. Thus, besides the contraception that the prolongation of the lactational period offers, it also aids with the baby’s health.
Hormonal contraception
This regards the use of oestrogen and progesterone-like compound hormones that are produced by a woman’s ovaries.
- Hormonal methods offer continuous contraception by blocking a woman’s ovulation.
- Women with a history of cardiovascular problems, diseases that affect the liver, breast cancer or hereditary thrombophilia, must choose other contraceptive methods
- Smoking and age beyond 35 years are additional prohibitive factors.
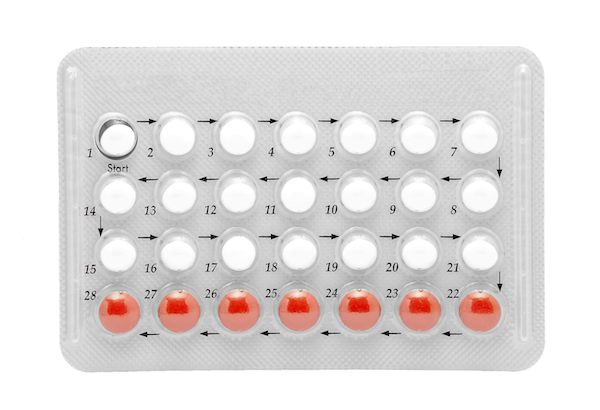
Oral contraceptive pill
Contraceptive pills contain compound oestrogens and progestogen. A woman who receives contraceptive pills has her cycle regulated at four weeks. If she adheres to the doctor’s instructions, the method is 99% successful.
Possible side-effects include nausea, dizziness, low mood, reduced libido, blood stains in between periods and fluid retention.
Rarely, hypertension, cardiovascular attacks and thrombosis may occur (smokers and women over the age of 35 or who suffer from thrombophilia). In addition, obesity, surgical operations and lack of exercise increase the possibility of thrombosis.
- The mini-pill that contains exclusively progestogen (progestogen-only contraceptive pill) is available, and this is also received daily.
If a woman forgets to take one pill, or does not take them at approximately the same time every day, or if she uses other medicines simultaneously, the contraceptive action is reduced and the possibility of pregnancy is increased.
Patch
Cutaneous (skin) patches release oestrogen and progestogen directly into the blood. They are placed on the hips or the lower abdomen (not the breasts) for three weeks. They contain a larger ratio of oestrogen than contraceptive pills creating, thus, a larger possibility for thrombosis. Their effectiveness is 92%, possibly less.
Vaginal ring (NuvaRing)
This is a flexible ring-shaped device with 5.4 diameter that the woman inserts in the vagina on her own. It contains oestrogen and progestogen that are released daily. It remains in this spot for three weeks and is removed after that so that menstruation can begin. If it is removed from the vagina for three hours or more, contraception will be ineffective. Besides the side-effects that are mentioned above, which concern other methods as well, there are possible symptoms of increased vaginal discharge, a risk of vaginitis and local irritation.
Injectable implants
These are the size of match, i.e. they are slim, small and flexible of rubber material and contain progestogen. They are placed on the inner side of the upper arm and slowly release the hormone. Their action lasts for three years and must be placed and removed via a minimally invasive surgical operation. For three to four days they cause local irritation and pain on the surgical site.
Possible side-effects include abnormal menstruation, dysmenorrhea (pathological pain during menstruation), acne, headaches, weight increase, breast tension, changes in mood and libido and hypertension. It is important that a woman attends regular gynaecological screening.
Intrauterine contraception (intrauterine devices, IUDs)
An IUD is a small plastic device with a metallic encasement, usually made of copper. It is placed in utero in a gynaecologist’s office or a in an obstetrics clinic. Commonly, anaesthesia is not necessary. It must always be removed be a gynaecologist.
Its contraceptive action is due to the change in the density of the cervical mucus, thus preventing the entry of sperm. What is more, it creates a non-friendly environment for the implantation of a fertilised ovum.
They are 98% effective.
Possible side-effects include pain, bleeding, salpingitis and, rarely, pelvic inflammation which may result to infertility.
Women with a history of extrauterine pregnancy, pelvic inflammation, un-investigated vaginal bleeding and fibromyomas that affect the inner part of the uterus must resort to other contraceptive methods.
There are hormonal IUDs (Mirena) which contain slow-releasing progestogen within the rubber and may remain in utero for five years.

Barrier methods
Barrier methods had an international dynamic come-back due to the fact that they offer satisfactory protection from unwanted pregnancies and, simultaneously, provide protection from sexually transmitted infections.
These methods are advantageous because:
- There are no systemic (body system) side-effects
- They are the sole substantial protection against AIDS and other venereal diseases.
- They are used only when necessary.
Condom
Male condom
It creates a barrier between the penis and the vagina during sexual intercourse.
It is usually made of latex or polyurethane.
Its purpose, on one hand, is to prevent pregnancy and, on the other hand, to prevent the transmission of sexually transmitted infections during intercourse.
They are one-use only and can be found in several forms: with lubricants, but also with spermicide for greater effectiveness.
Some people (the man or the woman) may be allergic to latex. In this case, polyurethane condoms do not cause any irritation.
Their effectiveness as a contraceptive method depends on proper use and varies between 85–98%. This is due to the fact that the condom may rip.
Couples who regularly use condoms during intercourse, greatly reduce the risk of catching sexually transmitted infections such as AIDS, Gonorrhoea, Human papillomavirus (HPV), Chlamydia, Syphilis.

Female condom

- A female condom is larger and wider than a male condom.
- They are made of polyurethane and are usually compatible with lubricants.
- The woman places the condom in the vagina on her own even long before sexual intercourse takes place.
- They are unpopular in comparison to male condoms due to the fact that they are more difficult to use, more expensive and with higher failure rates.
Diaphragms and cervical capsules
- The woman places them on her own a bit before sexual intercourse takes place and block access to the cervix.
- For additional safety, they are used in combination with spermicide creams.
- They are not felt during intercourse and this is one of their advantages. However, they do not protect from sexually transmitted infections (there is little protection when used in combination with spermicide creams) and women who chose this method must be experienced in placing them, in order to have the desired contraceptive effect.

Surgical contraception
Female sterilisation
Ligation of the fallopian tubes via several methods.
It can be done:
- Laparoscopically
- During Caesarian section
- Via laparotomy
- Male sterilisation
- Vasectomy
Emergency contraception
Emergency contraception, or next-day contraception, can be use by a woman who has had sexual intercourse without any protection during a possibly fertile period or in case the condom ripped. A hormone compound or progestogen-only is used with a success rate of 75–85%. In addition, an IUD can be used with a 99% success rate.
Nausea and vomiting are common side-effects. Moreover, atypical abdominal pain, headaches, dizziness and vaginal bleeding may occur.

It is essential that contraception is personalised. To find out which type best suits you, please contact us.
 English
English Ελληνικα
Ελληνικα



